Published on 20 February 2022
From a $200,000, fully-equipped soundproof booth, to a portable system that fits neatly in a suitcase: this could be the future of audiology.
Known as the boothless method, this innovation is indeed a timely one, as unaddressed hearing loss becomes increasingly a problem in Singapore’s greying society. In a 2018 national screening programme for seniors, some alarming statistics were revealed: 93% of seniors failed a hearing screening with some degree of hearing loss, and 61% of seniors with significant hearing loss.
While not a major health problem in itself, if unaddressed, hearing loss can lead to a host of problems. “What we find published in many, many studies is that if we don't address the hearing loss, there's a decreased quality of life,” said Prof William Hal Martin, an audiologist from the Department of Otolaryngology at the National University Hospital (NUH). He cited depression, anxiety, paranoia, social isolation, and increased risk of dementia and falls as possible consequences.
But many seniors are reluctant to seek help for their hearing issues. One reason could be due to the inconvenience. Up to recently, patients had to endure a number of referrals in order to see an audiologist – from the polyclinic, to an outpatient ENT clinic, and finally to an audiologist at a restructured hospital.
As such, there is an urgent need to make these services more accessible in the community.
“I think almost everybody I’ve talked to says, my mum or my dad has hearing loss, but they don't want to do anything about it,” shared Prof Martin. “And so we need to find out how we can care for our seniors.”
The boothless method, developed by the hearing research team at the NUS Yong Loo Lin School of Medicine (NUS Medicine) and led by Prof Martin, hopes to be a step in that direction. It aims to help overcome one of the biggest problems in doing hearing tests: the need for a sound-isolated booth.
The problem in question is ambient noise. Ambient noise can interfere with test results, making a patient’s hearing seem much worse than it really is. As a result, in order to get accurate results, hearing tests have conventionally been conducted in sound-isolated booths in hospitals.
But such booths run from $20,000 for a small, simple booth, to $200,000 for a full-sized one. “These are single use spaces, they're expensive, they take up a lot of room in hospitals, but they're not really useful for much of anything else,” explained Prof Martin, who is also Professor of Otolaryngology and Public Health at NUS Medicine. “So there's a limit to the number of test facilities that are available. And as a result, we get backups in the wait times, and crowding in the restructured hospitals.”
To eliminate the need for these test booths, the team spent a number of years to develop, evaluate and implement new hearing testing technology and protocols, with the result being the boothless audiometry protocol.
Compared to conventional, gold-standard testing, the team found that “they were clinically equivalent – the results were the same no matter which method we use, and we could even use it in [noisy situations],” said Prof Martin.
The boothless method has a number of advantages. Without the need for expensive soundproofing in rooms, it’s about 30% less expensive than conventional methods. It’s also more portable – all the required equipment can be fitted into a carry-on suitcase, and set up in any room, even if there’s ambient noise.
This means that audiology services can now be conducted not just in polyclinics and satellite clinics, but even in to home-bound patients, said Prof Martin.
“So this is really opening new horizons in the field of audiology,” he shared.

Bringing audiology to the community
The boothless method is being piloted in three community-based hearing clinics around Singapore: at Pioneer Polyclinic managed by NUH, as well as Tiong Bahru Community Health Centre and SGH Sleep Centre in SingHealth Tower.
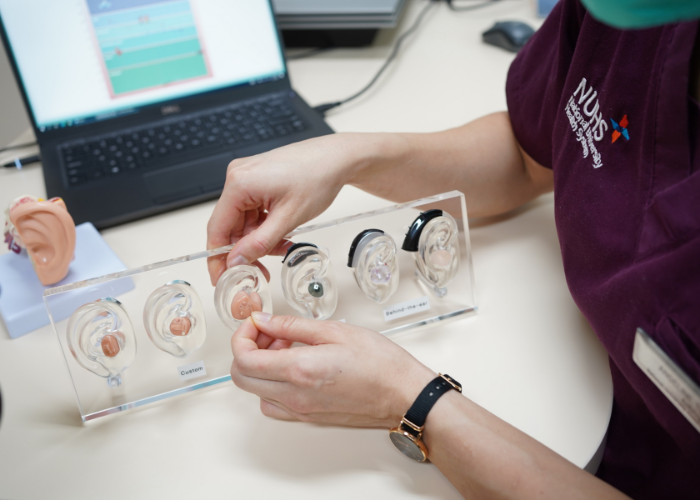
With these satellite clinics, “patients do not need to go all the way to the main campus [at NUH] to receive the full diagnostic and rehabilitation services,” said Dr Jenny Loo, Chief Audiologist at the Department of Otolaryngology, NUH.
In addition, these hearing clinics could also free up resources for restructured hospitals to focus on patients with more severe and complex hearing issues, said Mr Gopal Krishna Sarepaka, Senior Manager and Senior Principal Audiologist at the Singapore General Hospital (SGH) ENT Centre.
“We hope to be able to contain all these stable, elderly patients right here in the community,” he added. “Indirectly, these will also help with our wait times.”
A cultural barrier
However, some patients remain reluctant to seek help for their hearing problems.
In a previous study with the NUH Mobile Hearing Clinics, 73% of Singapore seniors said that they would never get their hearing tested. In addition, only about 5% of the people who would benefit from hearing aids actually ended up getting them.
“There's definitely a cultural obstacle to pursuing help for hearing loss that we see in Singapore. And we’re trying to understand it,” said Prof Martin. “They’ll blame it on costs, but through the Senior Mobility Fund and domestic subsidies, the cost of hearing aids is incredibly affordable. They talk about convenience – well, the Mobile Hearing Clinic has been driving in the neighborhoods providing services for a couple years now.
“So all of the excuses that are put forward to us don't seem to be real obstacles, there's another reluctance that may be much deeper,” he explained. “And we're starting to do research on this…but clearly, convenience and easy access is one of the issues that needs to be resolved.”
Another reason, said Dr Loo, could be the difficulty in getting used to hearing aids.
“Hearing loss is not so easily detected,” she said, “so most of the patients who actually come forward to get their hearing tested and who are willing to put on hearing aids, they’ve probably suffered from hearing problems for more than 10 years.”
As a result, the brain has already forgotten what environmental sounds are like – and when patients put on the hearing aids, they end up being overwhelmed, she added.
“Most of the time, patients actually need therapy sessions or progressive tuning of the hearing aids to adjust to them, because the brain has rewired itself…you want to bring the brain back to being alert to environmental sounds,” said Dr Loo.
Finally, there is the factor of visibility, said Mr Gopal. “Because it’s not a visible kind of disability, we do see a lot of the elderly who need some patient education,” he explained.
“In the audiology community, we’re quite aware of this problem. So we do a lot of awareness campaigns…and so I’m hoping that with all these things, acceptance of hearing aids will be better and acceptance of hearing loss will be a lot better.”


-(400-x-300-px).png?sfvrsn=19371fe8_1)

