Published on 4 July 2023
Patients suffering from obstructive sleep apnoea can now opt for a new treatment option known as hypoglossal nerve stimulation (HGNS) to help them breathe better while sleeping.
Do you frequently snore in your sleep?
If so, you might be suffering from obstructive sleep apnoea (OSA) – a serious sleep disorder that affects a person’s breathing and interrupts sleep.
According to a study, one in three Singaporeans suffer from OSA, which can cause daytime fatigue, headaches upon waking, sexual dysfunction and cognitive impairment.
Dangers of sleep apnoea
Untreated OSA is also associated with health problems such as hypertension, arrhythmias (irregular heartbeats), coronary artery disease, diabetes, and stroke. The risk of heart attacks and even death from any cause goes up with increased severity of OSA.
Those who suffer from OSA may experience symptoms such as gasping, choking, or temporary cessation of breathing during sleep.
“Witnessing these events can be very worrying for people who fear for their bed partner’s life,” said Dr Crystal Cheong, Consultant, Department of Otolaryngology, Head & Neck Surgery, National University Hospital (NUH) and NTFGH.
Treating sleep apnoea with CPAP
One of the most common ways of treating a patient with OSA is through the use of a continuous positive airway pressure (CPAP) machine during sleep, which delivers a constant stream of pressurised air into the nose, and sometimes mouth.
However, many patients find it uncomfortable to use CPAP as it involves an external device being strapped onto them. As such, while CPAP has long been considered the ‘gold standard’ for treating OSA, patients might prefer to try another option.
Dr Cheong explained, “Many treatment options apart from CPAP exist. The decision as to which treatment to use centres around the severity of the patient’s OSA and the patient’s preferences. Some patients may require combination therapy to get better.”
A new treatment option for OSA
Now, a new treatment could help patients with OSA breathe better while sleeping in comfort. Although recently introduced into Singapore, the treatment has been used by over 50,000 patients in the United States and Europe since 2014.

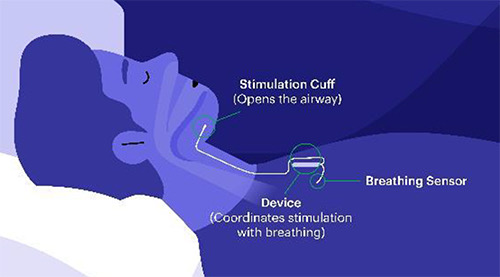
Known as hypoglossal nerve stimulation (HGNS) therapy, it involves implanting a small device in the neck and chest of the patient via a surgical procedure.
The device monitors the patient’s breathing during sleep, and delivers a mild electrical stimulation to move the tongue forward with each breath. This prevents the tongue from blocking the back of the throat, keeping the patient’s upper airway open and maintaining smooth airflow.
Elaborating on the merits of HGNS, which is now available at NUH, Dr Cheong said, “The implant is easy to use and comfortable to sleep with. The patients turn it on when they are ready to sleep, and turn it off when they are awake. Many seek out HGNS as they dislike the inconvenience and discomfort of having equipment over their face night after night, and are annoyed by tubing that can get entangled with their limbs or bedlinen.
“The process to put in the implant is a straightforward two-hour-long surgery that has a very manageable recovery. The patient is often able to go home on the same day of surgery and is expected to be able to eat and talk normally after surgery.”
Patients who undergo HGNS surgery are advised to avoid heavy lifting or excessive exercise for up to four weeks.
“Patients will have several follow-up visits in the first few months after surgery to review their healing, learn how to use the implant, and undergo a sleep study during which the implant is adjusted to the optimal setting for their breathing,” said Dr Cheong.
“Thereafter, if they have acclimated well and the implant is successful in controlling their OSA, they may return for an annual review.”
International studies have shown that approximately two in three patients on HGNS have significant reduction in their OSA and about one in three patients are cured of OSA.
However, not everyone who suffers from OSA is eligible for HGNS.
“The eligibility criteria for HGNS includes moderate to severe obstructive sleep apnoea and the inability to tolerate CPAP therapy,” Dr Cheong shared. “The patient must also undergo a brief examination called drug-induced sleep endoscopy to confirm that his/her upper airway collapse pattern is suitable for HGNS.”
Dr Cheong added that while there are several risks associated with HGNS, it is generally a safe and fuss-free procedure.
“An open and detailed discussion with the doctor is important, so that patients are aware of what to expect before and after surgery,” Dr Cheong said. “Our aim is to ensure the device is programmed optimally for each patient to have maximum benefit during sleep.
“As with any implant, infection, slight movement within the body where it is placed, and device malfunction are potential risks. Temporary tongue weakness following surgery has also been reported. Fortunately, these adverse effects are very uncommon based on studies conducted in thousands of patients, making it a viable alternative to CPAP therapy.”


