Published on 28 September 2022
Senior Staff Nurse Eve Ong takes us into NUHS@Home, where patients receive a mix of remote and at-home care.

As a Senior Staff Nurse at National University Health System (NUHS), Ms Ong ordinarily attends to patients who are frail with chronic diseases, or those who require end-of-life care.
But since 2 years ago when the NUHS@Home programme first started, Ms Ong also cares for patients who, instead of being hospitalised in the ward, are hospitalised at home instead. These include COVID-19 infected patients who are at high risk of severe disease, but want to recover at home.
These patients are admitted into NUHS@Home, where nurses and doctors check on them in virtual ‘ward rounds’ via teleconsultation, and ensure that they measure and report their vital signs regularly.
At the height of the pandemic, the team by the NUHS Regional Health System (RHS) and National University Hospital (NUH) Department of Medicine had over 100patients in their care.

Despite the bulk of their recovery being done at home, a number of patients may require some degree of medical treatment – such as blood tests, wound dressing, and the administration of medications to lower their risk of developing severe pneumonia.
Today, Ms Ong will be visiting two cancer patients. Such patients need to have their peripherally-inserted central catheter (PICC) lines flushed and dressed. This would ordinarily mean weekly visits to the hospital – but for patients in the virtual ward, nurses like Ms Ong visit them in their homes instead, to provide the necessary treatment as they recover from COVID-19.
With her calls done in the morning , Ms Ong prepares for this afternoon’s home visits. First, she drops by the pharmacy to pick up some heparinised saline, a flush solution for her cancer patients later.

In addition to her medical equipment, Ms Ong has to bring along supplies for infection control, including personal protective equipment (PPE). She packs all of these into her home care bag, which has a suitcase-style handle for easier transport.
Before heading off, she changes into her scrubs, which she wears under her PPE. After her visits, she’ll take a shower and change back out of her scrubs before going back to the office.
This is one of the multiple protocols in place to keep everyone safe from COVID-19 – an important factor for Ms Ong, who is a mother to three children.

It’s a busy day for Ms Ong, who makes her way to her first patient in a taxi. Typically, she has one to two home visits scheduled per day.
During the 30-minute-long ride, she manages to catch a short breather.

Before entering the patient’s home, Ms Ong dons her PPE.
“We need to be mindful and sensitive, and so we try to be discreet while gowning up,” she says.
“Many times, patients and their loved ones don’t want their neighbours to know that they’re infected with COVID-19.”

Ms Ong’s first patient of the day is Mdm Yang, a cancer patient under the care of the Covid Virtual Ward. This is her second visit to this patient’s home.
At the time of her visit, cancer patients like Mdm Yang had be isolated at home for 21 days. This protocol has since been reduced to 8 days.
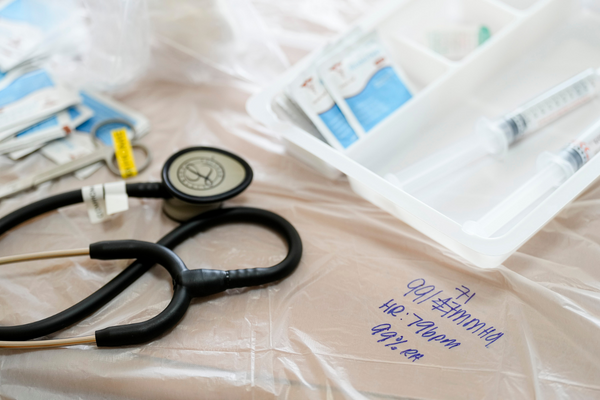
Before starting the treatment process, Ms Ong lays out a plastic sheet on a table, on which she places her medical equipment. She then takes Mdm Yang’s vitals: a standard start to every visit.

Even in the comfort of her own home, the quarantine is taking its toll on Mdm Yang. She repeatedly laments to Ms Ong on the struggles of not being able to head out during the festive period.
As Ms Ong starts to flush the PICC line, she strikes up a conversation with her patient on parenthood to engage her.

Changing and flushing the PICC line is a multi-step process. First, Ms Ong removes the old dressing and cleans the area. She then dresses the wound before flushing the catheter with normal and heparinised saline. Finally, she clamps it.
It’s a fairly quick process when done in the hospital. But when done in a home environment, alone and in full PPE, it takes Ms Ong 30 minutes to complete.

A little over an hour later, Ms Ong wraps up her home visit with Mdm Yang. She spends a while in the corridor removing and double-bagging the used PPE and supplies for disposal.
Despite the multiple protocols in place, Ms Ong says that things have improved since the start of the pandemic. Care delivery is more structured and streamlined.
“At the start of the NUHS@Home [programme], patients undergoing monoclonal antibody treatment would have to go to the hospital to receive the medication,” she says.
“But now, our nurses have been trained to administer the medication in the patient’s home.”
This also involves training to manage anaphylaxis (severe allergic reaction), one of the risks involved with the treatment

It’s time for the second patient. Ms Ong makes a quick call to the patient, Mr Aziz, from his void deck.
Mr Aziz was also undergoing chemotherapy when he was infected with COVID-19. Like Mdm Yang, his immunocompromised status means he is at risk of more severe disease, disqualifying him from the HRP.
The NUHS@Home is an in-between measure for such patients, who prefer not to be hospitalised or go to a community treatment facility, but who need monitoring and treatment.
This way, they can recover in the comfort of their home while still being monitored and receiving the necessary treatment.

Today marks Mr Aziz’s seventh day of infection. This is Ms Ong’s first visit to his home, to help him flush his PICC line.
As Singapore moves towards shifting care from hospital to community, NUHS@Home is expanding their bed capacity to continue to provide care for acute conditions at home.

Patients in the NUHS@Home must take and submit their vitals three times a day. These readings include their temperature, heart rate, and oxygen saturation, which are checked and monitored by care teams working round the clock.
Many patients are unfamiliar with equipment such as blood pressure monitors. They may also struggle with video calls.
“It can take around 45 minutes just to teach the patients how to take their blood pressure…step by step, because they don’t know how to use it,” she explains. “It takes lots of patience, but it’s satisfying when our patients learn to take charge of their health through technology.

The duration of each visit depends on the type of treatment a patient needs. Ms Ong’s longest home visit to date took two hours, during which she administered medication and performed blood-taking for a patient.
While tiring, this is a natural fit for Ms Ong, who started out working in wards. Her favourite part, she says, is the patients, who tend to be skewed to the geriatric population. “I like older adults,” she shares, “maybe because I was brought up by my grandmother when I was younger.”
To communicate with her older patients, Ms Ong speaks a variety of different languages and dialects: English, Mandarin, Hokkien, Teochew, and some Malay.

After 40 minutes in the patient’s non-air-conditioned home, sweat drips on Ms Ong’s glasses. Despite the heat and humidity, she chooses to have the fans turned off to prevent bacteria from entering the PICC line.

At 4.50pm, Ms Ong is done with her day’s home visits. She packs up and prepares to head back to NUH.
It’s been a long day, but a good one. “Many patients prefer to recover in their homes, where they can be near their families," she shares. “Especially for our cancer patients, who already spend so much time in the hospital…it’s not easy to be away from your loved ones.”
As such, despite the long hours and tiring work, “every day is meaningful and fulfilling,” says Ms Ong

While waiting for transport back to the hospital, she gets a call from a worried patient to clarify about infection control advice.
“Sometimes, patients will take the chance to consult us about their family member’s condition, even though they are not really under our care,” she says. “They’ll ask, ‘how about my mum?’ or ‘how about my son?’. So it’s not just the patients we have to manage.”
On the journey back, Ms Ong continues to work, updating her team on the events of today’s home visits.

Back in the hospital, Ms Ong cleans her bag and its contents with alcohol wipes. Her day isn’t over yet: she still has to take a shower and finish some administrative work before heading home.
As she cleans, several colleagues pass her as they make their home. They offer to help, but she demurs.
“It’s the heart that counts, and I’m thankful to have a team that always has my back,” she says. She adds that to keep spirits up and morale high, the team sometimes organises spontaneous activities, such as pizza days or coffee treats.
“If we were to take on everything, we’d probably [work] longer,” she says. “But we have a great care team to support us too, including medical staff, allied health, locums, and admin colleagues.




