Published on 1 November 2021
A novel drug delivery technique that could extend the lifespans of advanced cancer patients has been successfully introduced in Singapore, at the National University Hospital (NUH) and the National University Cancer Institute, Singapore (NCIS) – and for the first time in Asia.
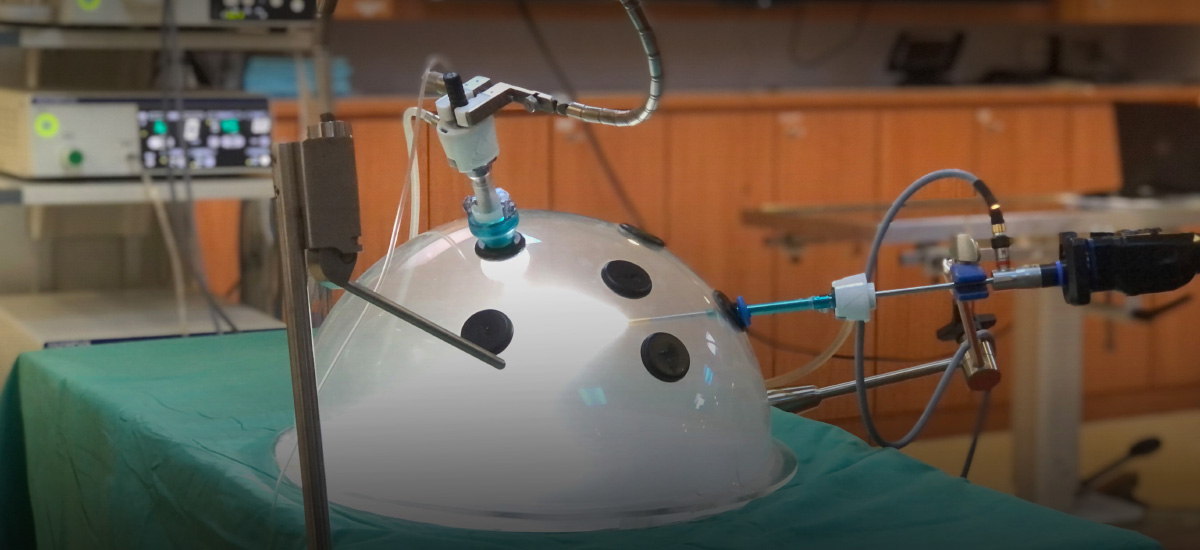
Known as pressurised intraperitoneal aerosol chemotherapy (PIPAC), the procedure targets cancers within the peritoneal cavity – where cancers tend to metastasise, or spread – in the abdomen, including colon, gastric, and ovarian cancer.
First, chemotherapy, an anti-cancer drug, is converted into fine droplets. A small ‘keyhole’ incision is then made in the abdomen, and the aerosolised chemotherapy solution is injected into the peritoneal cavity at high pressure, where it can act against the cancer cells.
The procedure has seen an approximately 60% response rate in patients. It could extend survival durations of end-stage cancer patients from between six to 12 months under conventional chemotherapy, to as much as 19 months, said Prof Jimmy So, Head and Senior Consultant at the NUH's Division of General Surgery (Upper Gastrointestinal Surgery).
Furthermore, the procedure causes few complications and side effects, allowing patients to preserve their quality of life.
This new approach could prove a recourse for end-stage cancer patients who suffer from numerous side effects and respond poorly to conventional chemotherapy, Prof So added.
“For this treatment…we try to relieve their symptoms. We try to control the cancer, with minimal side effects, for a long time,” said Dr Tan Hon Lyn, Consultant at the NCIS's Department of Haemotology-Oncology.
A better option for end-stage cancer patients
Currently, patients with peritoneal metastasis have a generally poor prognosis, Prof So said, calling it “an unsolved problem in oncology”.
For instance, they often suffer from severe symptoms, such as intestinal and kidney blockage, which are debilitating and very difficult to treat.
The conventional treatment of systemic chemotherapy – which is typically administered orally or intravenously – has also yielded poor results for such patients, he added.
This is because with systemic chemotherapy, the drug is unable to effectively penetrate the peritoneum.
In addition, side effects are usually severe due to high drug toxicity, because “the drug is distributed throughout the body”, explained Dr Kim Guowei, Consultant at NUH’s Division of General Surgery (Upper Gastrointestinal Surgery).
“As such, there may be systemic side effects, such as low blood count or feeling tired.”
For such patients, PIPAC could be a better, safer treatment option.
First, because it is injected into a targeted space, less of the drug is needed, and very little of it is able to escape into the blood system, said Dr Kim. This means there is less toxicity and fewer adverse side effects to contend with.
Second, due to the physical properties of gases, the chemotherapy can be distributed evenly within the abdominal cavity.
Third, as it is injected with pressure, the drug penetration will be deeper into the tumour tissue, allowing it to more effectively kill cancer cells.
There are other advantages as well. For instance, as it is a minimally invasive procedure, it can be carried out multiple times. The progress of the cancer can also be tracked through a camera system called a laparoscope during the procedure, to assess if the tumour is expanding further.
Future steps
Since it was introduced into the hospital in December 2016, NUHS has carried out 49 PIPAC procedures in 31 patients with zero mortalities. It is also the main training centre for PIPAC in Asia.
As it is still in clinical trials, the technique is currently being used exclusively on end-stage peritoneal cancer patients. However, positive results could mean the extension of the treatment to earlier-stage cancer patients – or even cancers in other parts of the body, said Prof So.
The team is also working on more studies to increase the technique’s effectiveness.
So far, they have successfully determined the optimal dosage of oxaliplatin – the chemotherapy drug currently used in PIPAC – in order to minimise side effects and maximise results. The study was published in the Clinical Cancer Research journal two months ago, and the guidelines have since been adopted in institutions worldwide.
They have also published a preclinical study examining if a paclitaxel – an alternative chemotherapy drug that is highly effective in stomach cancer – could also be safely used in PIPAC, said Prof So.
In addition, the team is working on first-in-human trials to see if PIPAC can be combined with systemic immunotherapy for even better results, he added.
“Peritoneal metastasis is a common problem in many patients with advanced cancer. Unfortunately, the current treatment results are unsatisfactory,” said Prof So.
“However, PIPAC is a safe, promising treatment for this disease that we hope can bring higher expectations and hope for our patients with advanced cancer.”
In consultation with Prof Jimmy So, Head and Senior Consultant, Division of General Surgery (Upper Gastrointestinal Surgery), NUH; Dr Tan Hon Lyn, Consultant, Department of Haemotology-Oncology, NCIS; and Dr Kim Guowei, Consultant, Division of General Surgery (Upper Gastrointestinal Surgery), NUH.