Published on 28 May 2024
A firsthand account of life with gastroesophageal reflux disease.
Many people would have at some point in their lives experienced acid reflux, which occurs when stomach acid travels up the esophagus. Some of the most common reasons for acid reflux include being a tad overzealous at the buffet table and consuming foods that are too acidic or fatty. This uncomfortable condition is usually no cause for concern and resolves itself within a couple of days. But for Mr Ow Sing Fuak, this condition is one that he has been battling every day for the past few years. Acid reflux that becomes chronic — as in this case — is known as gastroesophageal reflux disease (GERD).
According to Dr Kewin Siah, Senior Consultant, Division of Gastroenterology & Hepatology, Department of Medicine, National University Hospital (NUH), the individuals who face the highest risk of developing GERD include those who are obese as well as those who smoke or consume alcohol or caffeinated products regularly.
Other factors include hiatal hernia — which occurs when the upper part of the stomach bulges through the diaphragm into the chest cavity — and frequent consumption of certain medications like anticholinergics and non-steroidal anti-inflammatory drugs (NSAIDs).
First signs and the early stages
A former advertising professional, Mr Ow confesses to have been a heavy drinker of coffee due to the hectic nature and long hours of his job. “I drank coffee as if it was water,” quipped the 57-year-old. “I think I drank pretty much only coffee throughout the day during those times.”
Mr Ow recalled that his symptoms were mild when he first developed GERD more than 10 years ago. Besides feeling bloated, he also found himself burping frequently and experiencing heartburn – discomfort from stomach acids backing up into the esophagus. Although the doctor he visited prescribed antacids to lower the acidity levels in his stomach, Mr Ow quickly realised that the medication only provided temporary relief, as his symptoms kept resurfacing.
Subsequent visits to the doctor saw him walking away with stronger medication. He was also instructed to lose weight and abstain from spicy foods, and beverages like tea and coffee, all of which can exacerbate the condition.

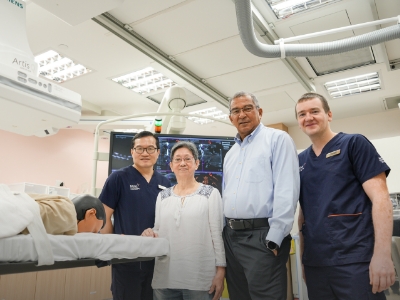
Mr Ow Sing Fuak, 57, now avoids caffeine, alcohol and spicy foods in order to manage his acid reflux symptoms.
A worsening physical and mental struggle
Despite being on medication, the situation nonetheless took a turn for the worse in 2018 when Mr Ow started experiencing severe heartburn episodes that left him struggling to stay on his feet. After receiving a referral to consult with specialists at the National University Hospital (NUH), he was treated with proton-pump inhibitors, which are more potent than the antacids he used to be given.
Unfortunately, his symptoms persisted and intensified over time. He even started getting anxiety attacks as a side effect of the disease. “I still remember experiencing heartburn and an anxiety attack when I was out in public alone,” he recalled. “It was a terrible experience. I had difficulty breathing. My whole body felt like it was cramping. I was on the verge of fainting.”
“The only thing I could do was to find a quiet spot away from the crowds to calm down. This is why I never leave home without medication these days.”
But things started looking up in 2019 when Dr Siah performed a gastroscopy on Mr Ow, which revealed erosive esophagitis and a small hiatus hernia. To address these issues, Dr Siah increased the proton-pump inhibitor doses and gave Mr Ow strict instructions to follow: completely avoid trigger foods, have smaller, more frequent meals, and shed a few more kilograms.
“Lifestyle modifications play a key role in reducing the risk of GERD,” Dr Siah explained. “Additionally, addressing underlying conditions like hiatal hernia and avoiding certain medications known to exacerbate GERD can also help mitigate risk.”
Mr Ow acknowledged that it has not been easy dealing with his condition. In fact, he admitted that it took him three years to accept the fact that he can no longer go about life like he used to.
Managing the disease long-term
Today, Mr Ow never leaves home without a small bag that contains no less than six medications. Ingesting medicine has become part and parcel of life. Tucked away in a corner of his home is not one or two bottles of antacid products, which is used to treat heartburn and indigestion relief — he has four cartons of the medicine.
Even his journey to losing weight was affected by GERD. “There was a point where I could not even run outdoors because the heat triggered the symptoms,” he said. “All I could do was walk on the treadmill at home.”
Regarding the reason behind this, Dr Siah explained that heat stress or higher temperatures have the potential to exacerbate symptoms of GERD due to increased perspiration and dehydration. “To address this, GERD patients should stay hydrated, avoid large meals before outdoor activities in hot weather, and manage stress levels, which can worsen the symptoms.”
While GERD remains a concern, Mr Ow now experiences symptoms far less frequently due to his adoption of a new lifestyle. Thanks to the 45-minute outdoor walks he takes two days a week and a healthier diet that is devoid of spicy and fatty foods, he now weighs 15 kg lighter than before. He has also completely given up on coffee and tea. Even carbonated beverages have been blacklisted.
According to Dr Siah, the latest assessment of Mr Ow’s condition suggests that there is a possibility of reducing his medication dosage, which would mark a milestone in his journey toward sustained well-being.
“I hope that more people will understand GERD through this sharing of my experiences. I want them to know that the condition of our gut affects much more than just the digestive system — it can impact the entire body and even our mental health,” he said. “To those who have this condition, don’t lose hope. The key to getting better is watching what you eat and being patient.”
In consultation with Dr Kewin Siah, Senior Consultant, Division of Gastroenterology & Hepatology, Department of Medicine, NUH.