Published on 15 October 2021
Each day, our immune system fights an ongoing battle with pathogens. But when medical conditions or treatments take down our defenses, it causes neutropenia.
Neutropenia (noo-troh-PEE-nee-uh) is one of the dreaded side effects of chemotherapy; it increases the risk of infections and serious illness, making it a medical emergency. With no obvious external signs – except maybe a fever – it is important to keep an eye out for this silent condition.
Neutropenia is a condition where the number of white blood cells (called neutrophils) drops to such a low level that the body becomes unable to fend off any germs. Neutrophils are an important component of white blood cells and the body’s immune defences. Without sufficient neutrophils to fight, one becomes vulnerable to infections, particularly those caused by bacteria and fungi.
According to Dr Frances Yeap, Consultant, Paediatric Haematology and Oncology, Paediatrics, Khoo Teck Puat - National University Children's Medical Institute, National University Hospital (NUH) and Consultant, Paediatric Haematology and Oncology, National University Cancer Institute, Singapore (NCIS), this condition is caused by many factors. It can be inherited or congenital and can also be caused by drugs, cancer, infection, autoimmune disease or nutritional deficiencies. Chemotherapy is one of the most common causes of neutropenia.
A risky side effect of chemo
Dr Yeap explained that neutropenia is especially common during cancer treatment. “Most Chemotherapeutic agents are ‘blind’,” she said, “It is a cytotoxic agent that kills cells, regardless whether they are good or bad, including blood cells.” Many other drugs such as antibiotics, immunosuppressant can also cause neutropenia.
It is typical for white blood cell counts to dip about seven to 14 days after the session, depending on the chemo used. This dip in immunity may be asymptomatic. However, in some cases, it may cause pain on swallowing, gum pain, weak nails as well as recurrent skin, sinus and ear infections. It also increases the risk of pneumonia and the risk of serious infection (sepsis) for those with central lines or implants.
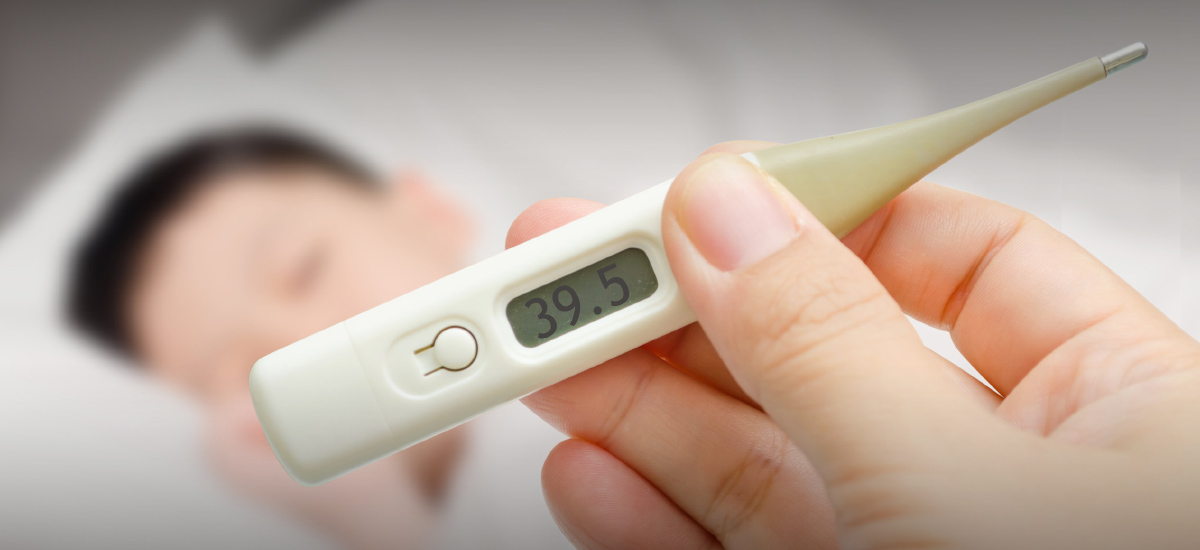
Fever is usually one of the more common symptoms. Dr Yeap highlighted that this type of fever requires urgent medical care in those who have recently had chemotherapy because it can escalate swiftly. “Neutropenic fever may resolve quickly with no major comorbidity, but it is a medical emergency as these patients can become septic and have overwhelming infections very quickly.”
Extra precaution needed
For this reason, hygiene and infection control measures are important to keep patients safe, particularly during periods of neutropenia, said Dr Yeap. Close temperature monitoring is also a helpful way to spot any early signs of fever.
Precautions to take include:
Scrupulous hand and daily hygiene, including oral hygiene
Using lotion after showering to prevent dry and cracked skin
Avoiding crowded places
Limiting contact with people, especially if they are sick
Ensuring fish, meat and eggs are cooked through
Avoiding raw foods
Not sharing food and eating utensils
Keeping central lines, implants, stomas or plugs clean
Tackling neutropenia
How neutropenia is treated depends on its causes and severity. Some types of neutropenia do not require treatment especially if these occur in a well child or person.
If the period of low immunity is expected to be prolonged, Dr Yeap said that a preventive course of antibiotics may be prescribed. Other drugs can also be given to stimulate the bone marrow to produce more white blood cells. If this is not effective and there is a risk of overwhelming infection, an infusion of white blood cells may be needed. In Bone Marrow Failure and other immunodeficiency where neutropenia may be part of the problem- a Bone Marrow Transplant is the only curative option.
While neutropenia can be challenging to prevent, precautions and treatments can make it easier to manage. Patients are monitored carefully with blood tests to track their blood counts so that early intervention or specialist treatment by a haematologist can be initiated if required. At NCIS, patient education and support are important part of treatment plans so as to achieve the best outcomes for patients.
In consultation with Dr Frances Yeap, Consultant, Paediatric Haematology and Oncology, Paediatrics, Khoo Teck Puat - National University Children's Medical Institute, National University Hospital and Consultant, Paediatric Haematology and Oncology, National University Cancer Institute, Singapore.